What is the average VA rating for migraines? Specifically, the 30 percent disability rating for migraine headaches can be broken down into three main components: (1) characteristic; (2) prostrating; and (3) average of once a month over the last several months. In this case, characteristic essentially means “typical”.
How do I get 50 VA disability for migraines?
VA Rating Criteria for Migraine Headaches
- 50% – with very frequent completely prostrating and prolonged attacks productive of severe economic inadaptability.
- 30% – with characteristic prostrating attacks occurring on an average of once a month over the last several months.
Is it hard to get VA disability for migraines? The maximum VA rating for migraine headaches is 50 percent under 38 C.F.R. 4.124a Schedule for rating disabilities with VA diagnostic code 8100, under Neurological Conditions and Convulsive Disorders. VA also rates migraines at 0%, 10%, and 30% for Veterans suffering from migraines due to an in-service incident.
What VA disabilities are secondary to migraines? There may also be secondary comorbidities such as neck, eye, or back injuries, fibromyalgia, and mental health issues. There can also be other secondary issues from the migraines such as sleep disorders, sleep apnea, chronic mental health issues such as depression and post-traumatic stress disorder.
What is the average VA rating for migraines? – Additional Questions
How do you prove migraines?
There’s no specific test to diagnose migraines. For an accurate diagnosis to be made, a GP must identify a pattern of recurring headaches along with the associated symptoms. Migraines can be unpredictable, sometimes occurring without the other symptoms. Obtaining an accurate diagnosis can sometimes take time.
Is there a C&P exam for migraines?
A veteran with suspected migraines should consult a neurologist who can make the appropriate diagnosis based on medical history, symptoms, and the results of a physical and neurological examination. A Compensation & Pension (C&P) exam will be scheduled when the VA receives your application for disability benefits.
What are VA secondary conditions?
What is VA Secondary Service Connection? This means that a service-connected illness or injury caused another illness, mental health condition or injury. For example, diabetes is one of the most common service-connected illnesses.
Can sleep apnea be secondary to migraines?
Sleep Apnea Secondary to Migraines
Sleep apnea, like insomnia, is a sleep disorder that can be connected to migraines. Sleep apnea is a serious condition in which a person’s breathing is repeatedly interrupted throughout the night.
Can migraines be secondary to tinnitus?
According to the American Migraine Foundation, there is a strong relationship between tinnitus and migraine headaches. Specifically, about 27 percent of individuals with tinnitus also suffer from migraines. Some individuals also report a worsening in tinnitus symptoms during migraine attacks.
Can migraines be secondary to PTSD?
For example, a veteran’s service-connected PTSD may later cause migraine headaches. In this case, the veteran’s migraines may warrant secondary service connection if they are the result of their service-connected PTSD.
What does a PTSD headache feel like?
Symptoms of post-traumatic headache can include sensitivity to light and noise, nausea, dizziness, vomiting, insomnia, poor concentration, fatigue and personality changes like depression or nervousness. The headache might also have a pulsating quality that worsens with activity.
Can head trauma cause chronic migraines?
When a serious injury occurs to the head, brain and/or neck, the risk for long-term complications is significant. In particular, headaches and migraine attacks develop regularly after traumatic brain injuries (regardless of severity), with estimates of prevalence between 58-81% of patients.
What is a post-traumatic migraine?
Post-traumatic headache (PTHA) is defined as a secondary headache that develops within 7 days after head trauma (or after regaining consciousness following head trauma).
Can PTSD and depression cause migraines?
Psychiatric disorders including depression, anxiety, and PTSD are associated with migraine, says Mueller. “People who have these conditions are more likely to experience migraine.
What can trigger migraines?
Bright or flashing lights can induce migraines, as can loud sounds. Strong smells — such as perfume, paint thinner, secondhand smoke and others — trigger migraines in some people. Sleep changes. Missing sleep or getting too much sleep can trigger migraines in some people.
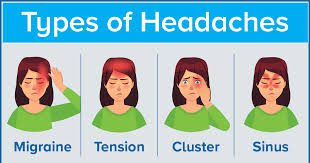
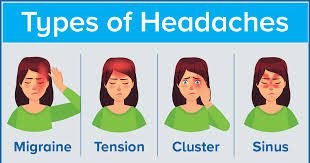
What are the 3 types of migraines?
The most common are migraine with aura (also known as a classic migraine) and migraine without aura (or common migraine). Other types include: Menstrual migraine.
What does a migraine do to your brain?
But during a migraine, these stimuli feel like an all-out assault. The result: The brain produces an outsize reaction to the trigger, its electrical system (mis)firing on all cylinders. This electrical activity causes a change in blood flow to the brain, which in turn affects the brain’s nerves, causing pain.
What is considered a chronic migraine?
Chronic migraine, a condition characterized by the experience of migrainous headache on at least 15 days per month, is highly disabling. Patients with chronic migraine present to primary care, are often referred for management to secondary care, and make up a large proportion of patients in specialist headache clinics.
How many migraines a month is too many?
Most people who are prone to migraines get a painful attack once or twice a month. But if you have the condition known as chronic migraine, you get headaches much more often — 15 or more days a month for at least 3 months.. These frequent and severe attacks can make living a normal life a challenge.
Are migraines a mental illness?
Migraine is a highly prevalent and disabling neurological disorder which is commonly linked with a broad range of psychiatric comorbidities, especially among subjects with migraine with aura or chronic migraine.
How long is too long for a migraine?
How long is too long? If a migraine headache lasts longer than 72 hours without responding to regular migraine medication, the person may need additional treatment. Anyone who has experienced this pain for longer than 3 days should speak with a doctor as soon as they can.