What is nerve decompression surgery for migraines? Nerve decompression surgery or migraine surgery strategically reduces pressure on the nerves to relieve migraine pain. In turn, it could reduce other symptoms, such as nausea, light sensitivity, fatigue, loss of appetite, abdominal pain, and dizziness.
How successful is occipital nerve decompression surgery? Many patients who undergo nerve decompression surgery have successful outcomes. In one study, 89.5% of nerve decompression surgery patients had complete resolution of headaches, while an additional 6.6% experienced significant relief and no longer needed additional treatment for head or neck pain.
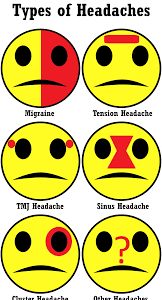
Who is a candidate for migraine surgery? In general, you may be a good candidate for migraine surgery if: You have been diagnosed with migraines or occipital neuralgia by a neurologist (not all headaches are migraines) You have tried several therapies (behavioral, medications) without success. You are physically healthy.
How much does nerve decompression surgery cost? RESULTS: The mean cost of peripheral nerve decompression surgery was $10,303 with an effectiveness of 7.06, whereas the mean cost of long-term, targeted BoNTA was $36,071 with an effectiveness of 6.34. Decompression surgery is more effective and less costly over the time horizon of the model.
What is nerve decompression surgery for migraines? – Additional Questions
How long does it take for nerves to heal after decompression surgery?
It will take about 4 to 6 weeks for you to reach your expected level of mobility and function (this will depend on the severity of your condition and symptoms before the operation). When you wake up after lumbar decompression surgery, your back may feel sore and you’ll probably be attached to 1 or more tubes.
How long is nerve decompression surgery?
Nerve Decompression / Neurolysis generally takes less than one-hour per surgical site and can be performed under general or wide awake local anesthesia. After surgery, the surgical area is wrapped in a soft dressing.
What is the cost of microvascular decompression surgery?
Forty-eight of these patients underwent microvascular decompression (MVD), 39 underwent stereotactic radiosurgery (SRS) and seven underwent percutaneous stereotaxic rhizotomy (PSR). The researchers reported that the average weighted cost of surgery was about $40,000 for MVD, $38,000 for SRS and $3,900 for PSR.
What is nerve decompression surgery?
Nerve decompression surgery is any operation to alleviate pressure on a nerve. Some nerves are more prone to compression than others due to the surrounding skeletal structure.
How often should you do spinal decompression?
How Often to Do Spinal Decompression? Typically, you will undergo 2-5 spinal decompression sessions per week, for four to six weeks. That’s 12-20 appointments before you can experience long-lasting pain relief.
When does a pinched nerve need surgery?
Surgery. If the pinched nerve doesn’t improve after several weeks to a few months with conservative treatments, your doctor may recommend surgery to take pressure off the nerve.
What is the success rate of pinched nerve surgery?
According to Spine-Health, the success rate of pinched nerve surgery is high, with approximately 90 percent of patients experiencing relief of pain. A majority of patients with acute or severe back pain can benefit more from a microdiscectomy or laminectomy.
Can a pinched nerve be detected with an MRI?
MRI scans which show soft tissues, such as nerves and discs, are generally preferred over CT scans which show bony elements. Advanced imaging can show exactly which nerve or nerves are being pinched and what is causing the nerve to be pinched.
How do they do surgery on a pinched nerve?
During foraminoplasty, a spinal surgeon will make an incision in the neck or back, depending on the location of your pinched nerves. Next, the spinal surgeon can widen the intervertebral foramen to remove any blockages or causes of compression surrounding a nerve.
How serious is spinal decompression surgery?
Death. As with all types of surgery, there’s a risk of dying during or after lumbar decompression surgery, although this is rare. A blood clot, a bad reaction to the anaesthetic and blood loss can all be life-threatening.
Can a pinched nerve become permanent damage?
Can a pinched nerve become permanent? The answer is most of the time a pinched nerve will get better with rest and over-the-counter medications. It can, however, become a chronic condition, so you should see a doctor if you don’t see improvement within a few days.
What will a neurologist do for pinched nerve?
It is recommended you see a board-certified neurologist if you suspect you have a pinched nerve. Your neurologist can relieve numbness and tingling by reducing the pressure on your nerves using one of the many neuropathy treatment options available.
Can a pinched nerve affect the brain?
Pinched Nerves in the Brain, Neck and Back
The nerve compression results in pain and other symptoms that can limit the crucial functioning of these nerves. This can disrupt the appropriate signals to control the muscles of the body.
What happens if nerve pain is left untreated?
Complications of peripheral neuropathy
If the underlying cause of peripheral neuropathy is not treated, you may be at risk of developing potentially serious complications, such as a foot ulcer that becomes infected. This can lead to gangrene if untreated, and in severe cases may mean the foot has to be amputated.
How long can a nerve be compressed before permanent damage?
Severe nerve compression that lasts more than six weeks can cause permanent muscle loss and nerve damage. You should see your healthcare provider early about symptoms so you can start the appropriate treatment.
Why is nerve pain worse at night?
At night our body temperature fluctuates and goes down a bit. Most people tend to sleep in a cooler room as well. The thought is that damaged nerves might interpret the temperature change as pain or tingling, which can heighten the sense of neuropathy.
What are the symptoms of brain nerve damage?
Cranial nerve damage may result in:
- Paralysis of facial muscles or losing sensation in the face.
- Loss of or altered sense of smell or taste.
- Loss of vision or double vision.
- Swallowing problems.
- Dizziness.
- Ringing in the ear.
- Hearing loss.