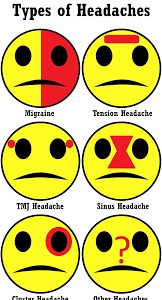
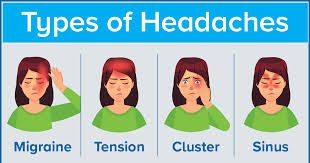
What type of headache does COVID-19 cause, and how does it compare to migraine? In some patients, the severe headache of COVID-19 only lasts a few days, while in others, it can last up to months. It is presenting mostly as a whole-head, severe-pressure pain. It’s different than migraine, which by definition is unilateral throbbing with sensitivity to light or sound, or nausea.
How long does headache last in COVID-19 patients? In some patients, the severe headache of COVID-19 only lasts a few days, while in others, it can last up to months. It is presenting mostly as a whole-head, severe-pressure pain. It’s different than migraine, which by definition is unilateral throbbing with sensitivity to light or sound, or nausea.
What can I take for a headache from COVID-19? If youre having headaches from COVID-19 illness, you can: Take over-the-counter pain relievers. Its safe to take both ibuprofen (Advil) and acetaminophen (Tylenol) for COVID-19 symptoms, including headaches.
What are some of the post-COVID symptoms?
Patients with COVID-19 were significantly more likely than were those without to develop the following assessed post-COVID symptoms: smell and taste disturbances (aHR = 1.17), circulatory signs and symptoms (1.07), malaise and fatigue (1.05), and musculoskeletal pain (1.02) (Table 2).
What type of headache does COVID-19 cause, and how does it compare to migraine? – Additional Questions
What are Post-COVID conditions or Long COVID?
Post-COVID conditions (PCC, or Long COVID) are a wide range of new, returning, or ongoing health problems people can experience four or more weeks after first being infected with the virus that causes COVID-19.
What are some of the symptoms of the long haulers from COVID-19?
People with long COVID, or “long-haulers,” are COVID-19 survivors but they have persistent symptoms such as shortness of breath, fatigue, headaches, palpitations, and impairments in mental health and cognition.
How long do lingering symptoms last after COVID-19?
Symptoms. People with post-COVID conditions (or long COVID) may experience many symptoms. People with post-COVID conditions can have a wide range of symptoms that can last more than four weeks or even months after infection. Sometimes the symptoms can even go away or come back again.
What is long COVID-19?
Some people who have been infected with the virus that causes COVID-19 can experience long-term effects from their infection, known as post-COVID conditions (PCC) or long COVID.
Which organ system is most often affected by COVID-19?
COVID-19 is a disease caused by SARS-CoV-2 that can trigger what doctors call a respiratory tract infection. It can affect your upper respiratory tract (sinuses, nose, and throat) or lower respiratory tract (windpipe and lungs).
What organs could be affected by the long term effects of a severe COVID-19 disease?
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isnt clear how long these effects might last.
How does COVID-19 affect the heart and lungs?
SARS-CoV-2, the virus that causes COVID-19, most commonly affects the lungs but It can also lead to serious heart problems. Lung damage caused by the virus prevents oxygen from reaching the heart muscle, which in turn damages the heart tissue and prevents it from getting oxygen to other tissues.
Can the COVID-19 virus affect your kidneys?
Does COVID-19 affect the kidneys? It can. In addition to attacking the lungs, the coronavirus that causes COVID-19 — officially called SARS-CoV-2 — also can cause severe and lasting harm in other organs, including the heart and kidneys.
Can kidneys recover after COVID-19?
Can kidneys recover after COVID-19? Sperati says, “Patients with acute kidney injury due to COVID-19 who do not require dialysis will have better outcomes than those who need dialysis, and we have seen patients at Johns Hopkins who recover kidney function.
Can COVID-19 affect your organs?
People who had severe illness with COVID-19 might experience organ damage affecting the heart, kidneys, skin and brain. Inflammation and problems with the immune system can also happen. It isn’t clear how long these effects might last.
How much water should you drink a day if you have the coronavirus disease?
“If you’re at home treating COVID-19 symptoms, remember to stay hydrated,” Dr. Mehta says. “Drink at least 64 to 70 ounces of water every day.”
What is a good way to hydrate if I have COVID-19?
Stay hydrated. “Drink at least 64 to 70 ounces of water every day.” To replace lost electrolytes — which can happen through fever-induced sweating, for example — you may want to consider a half-and-half mixture of water and an electrolyte-rich sports drink, such as Gatorade or Powerade.
What kind of food should I eat if I have COVID-19?
If you aren’t nauseous, but you’re experiencing an altered sense of taste, things might not taste great—so you might not care about what you eat. Some might lean toward easy, processed foods or sugar. But it’s important to eat healthy foods, as nourishing your body will help you recuperate.
What not to eat during the COVID-19 pandemic?
Avoid foods that are high in salt and sugar. Limit the number of soft drinks and other drinks that are high in sugar. Instead of sweet snacks like cookies, cake, and candy, choose fresh fruits.
What are some of the most effective foods to reduce inflammation during the COVID-19 pandemic?
Foods to help you reduce inflammation include: Apples, berries, tomatoes, celery and onions (veggies and fruits) Yogurt, sauerkraut and kombucha (probiotics) Salmon, walnuts and chia seeds (omega-3 fatty acids)
Does vitamin D affect COVID-19?
Vitamin D plays a role in the body’s immune system and is known to enhance the function of immune cells. In this case, Vitamin D inhibits some of the inflammation that can make COVID-19 more severe.
Are you still contagious with COVID-19 after 5 days?
Chan School of Public Health in Boston, Massachusetts, who has worked on similar PCR-based studies of infectiousness, agrees that ten days is a useful rule of thumb for when people should no longer be contagious. But he cautions that a small number of people could still be infectious beyond that point.