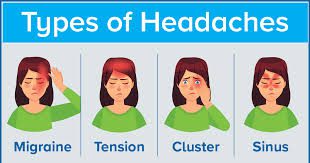
Can Sjogren’s syndrome cause migraines? Some of the most common types of headaches include tension type headaches, migraines (with and without aura), and cluster headaches. Headaches are common in Sjögren’s, estimated to occur in roughly 50 to 75% of patients.
What autoimmune disease causes migraines?
Migraine often adversely affects autoimmune disease, and autoimmunity often adversely affects Migraine.
Autoimmune Diseases
- Multiple Sclerosis.
- Systemic Lupus Erythematosus (SLE) aka Lupus.
- Sjogren’s Syndrome.
- Rheumatoid Arthritis.
- Grave’s Disease.
- Hashimoto’s Disease.
- Ankylosing Spondylitis.
- Giant Cell Arteritis.
What are the hallmark symptoms of Sjogren’s syndrome? The hallmark symptoms of Sjögren’s syndrome are extreme dry eyes and mouth. Some people also experience joint pain, swelling and/or stiffness. Sjögren’s syndrome that occurs by itself is called primary Sjögren’s syndrome.
Are migraines part of autoimmune disease? Recent experimental and supportive epidemiological evidences provide sufficient indications towards migraine being an autoimmune disorder and they are discussed in detail below.
Can Sjogren’s syndrome cause migraines? – Additional Questions
Are migraines an inflammatory response?
Migraines are a form of neuroinflammation that is set into motion by interactions between brain cells, nervous system cells, blood vessels and systemic inflammation. While we can’t promise that an anti-inflammatory diet will keep migraines at bay, it can boost your overall health and potentially ease migraine symptoms.
What can daily migraines mean?
Conditions that might cause nonprimary chronic daily headaches include: Inflammation or other problems with the blood vessels in and around the brain, including stroke. Infections, such as meningitis. Intracranial pressure that’s either too high or too low. Brain tumor.
Is migraine a symptom of lupus?
Headache. About 20% of patients with lupus have migraine-like headaches. These headaches are different from “lupus headaches,” which are due to active lupus and require a lumbar puncture (spinal tap) or blood vessel study (MRA or CT-angiogram) for diagnosis.
Is there a link between migraines and rheumatoid arthritis?
Researchers say there appears to be a dual connection between rheumatoid arthritis and migraine. They say people who have migraine are more likely to develop rheumatoid arthritis, and people with this type of arthritis are more likely to develop migraine.
What are some autoimmune neurological disorders?
Autoimmune Neurological Disorders
- Multiple Sclerosis. An MRI image showing areas of inflammation and scarring in the brain of an MS patient.
- Transverse Myelitis.
- Optic Neuritis.
- Neuromyelitis Optica.
- Acute disseminated encephalomyelitis.
- Autoimmune or Paraneoplastic Encephalitis.
- Rare Neuroimmunological conditions.
- Spasticity.
Are migraines related to other diseases?
The comorbid illnesses in patients with migraine include stroke, sub-clinical vascular brain lesions, coronary heart disease, hypertension, patent foramen ovale, psychiatric diseases (depression, anxiety, bipolar disorder, panic disorder, and suicide), restless legs syndrome, epilepsy and asthma.
Who is more prone to migraines?
Women are three times more likely than men to have migraines. Hormonal changes. For women who have migraines, headaches might begin just before or shortly after onset of menstruation. They might also change during pregnancy or menopause.
Do migraines count as a neurological disorder?
A migraine is a common neurological disease that causes a variety of symptoms, most notably a throbbing, pulsing headache on one side of your head. Your migraine will likely get worse with physical activity, lights, sounds or smells. It may last at least four hours or even days.
What are the 3 types of migraines?
The most common are migraine with aura (also known as a classic migraine) and migraine without aura (or common migraine). Other types include: Menstrual migraine.
What is a silent migraine?
If you have a silent migraine, it means you get any of the typical migraine symptoms except for one: pain. Your doctor may suggest medications or devices that can treat the problem. You can also help yourself by avoiding your migraine triggers.
What is the fastest way to cure a migraine?
In this Article
- Try a Cold Pack.
- Use a Heating Pad or Hot Compress.
- Ease Pressure on Your Scalp or Head.
- Dim the Lights.
- Try Not to Chew.
- Hydrate.
- Get Some Caffeine.
- Practice Relaxation.
What is an ocular migraine like?
Retinal migraine (ocular migraine) is an eye condition that causes brief attacks of blindness or visual problems like flashing lights in 1 eye. These episodes can be frightening, but in most cases they’re harmless and shortlived, and eyesight goes back to normal afterwards.
Is ocular migraine a mini stroke?
The bottom line. Ocular migraine, or migraine with aura, and stroke are two different conditions. Having an attack doesn’t mean you’re having a stroke or are about to have one.
What kind of doctor should I see for ocular migraine?
Ophthalmologist or optometrist.
You might be referred to an eye specialist if, along with your migraine, you have what’s called aura. This can include: Changes in your vision like blind spots or flashes of light.
Why am I suddenly getting ocular migraines?
Harsh lighting, long screen time, other visual strain, stress, dehydration, food additives, and other causes all may trigger an ocular migraine, a subtype that focuses in the eye and causes vision changes.
What is the difference between an ocular migraine and a retinal migraine?
People may use the terms ocular migraine and retinal migraine to mean the same thing, but there are some important differences. An ocular migraine generally occurs in both eyes. A retinal migraine is rare and tends to occur in just one eye, when vessels that supply the eye with blood narrow.
What causes zig zag lights in vision?
Kaleidoscopic vision is most often caused by a type of migraine headache known as a visual or ocular migraine. A visual migraine occurs when nerve cells in the part of your brain responsible for vision begin firing erratically. It generally passes in 10 to 30 minutes.